Hungary respiratory season worsens at end of the reporting period

Looking at the number of influenza-like illness cases per 100,000 people, we can see that the peak in the 2024/25 season was rather high. Only the peaks in the 2016/17 and 2014/15 seasons were higher; the former by quite a lot and the latter by a smaller amount.

Interestingly, the number of people visiting the doctor with an acute respiratory illness increased for the second week in a row, both in absolute terms and per 100,000 people. While this does not necessarily indicate that the respiratory season will continue to worsen, it is impossible to tell because the NNGYK stops publishing data after the 20th week.

As mentioned above the respiratory season peaked a lot higher than in the previous two seasons when looking at ARI numbers per 100,000 inhabitants.

The peak was higher in absolute terms, too, but not dramatically. However, in terms of ILI numbers, this respiratory season was much worse than the previous two in the first ten weeks of 2025.

The number of samples tested exceeded 9,200, which compares with less than 7,200 last year and less than 4,400 a year before that.
The cumulated number of human metapneumovirus (HMPV) cases was largely the same in the current season as in the previous one up until the fourth week this year, but then it started to rise rapidly, and by the end of the 20th week it reached 270 against 182 a year earlier.

The Covid-19 positivity rate peaked at 34.4% on the 40th week of 2024, but remained lower than in the previous two respiratory seasons all the way.

The influenza positivity rate was higher than in the previous two respiratory seasons between the 47th week of 2024 and the 8th week in 2025.

The RSV positivity rate took to the lead on the 9th week and remained there practically through to the end of the 20th week.

Overall, in terms of hospitalisations, this season did not differ greatly from the previous two. If anything, it was definitely milder than in 2022/23 and for some weeks milder than in 2023/24.

As for the reasons behind hospitalisations, influenza and RSV infections kept vying for the first place, except for about ten weeks at the start of the season when coronavirus was the main culprit. After the 11th week, the main reason why people had to be hospitalised with severe acute respiratory infection (SARI) was RSV.

Compared to the previous two respiratory seasons, influenza infection definitely caused more trouble, and RSV infections made life difficult for more people than in 2022/23 and 2023/24 after the 11th week, while Covid was behind a smaller proportion of SARI-related hospitalisations.



The age distribution of the number of ARI and ILI cases shows that the youngest people were the most affected throughout almost the entire respiratory season.


The youngest age group was also the most affected in terms of hospitalisations for RSV infection, while the share of Covid-linked hospitalisations was the highest among those aged 60 years and over.

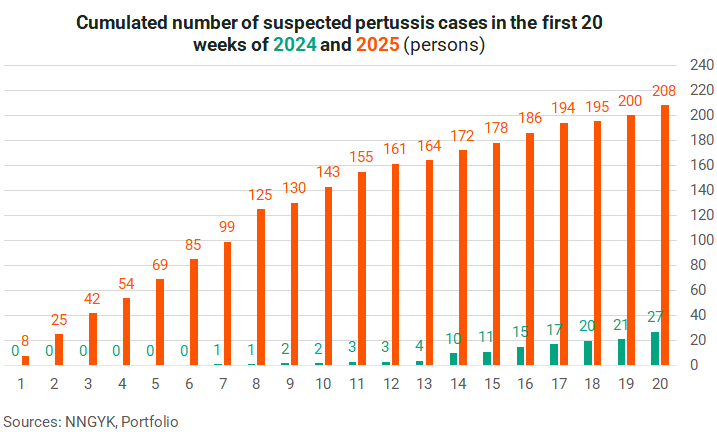
The number of cases of pertussis is also rising. Based on data from the first 20 weeks, it would be a miracle if a new record were not reached this year. Infants are the most affected with nearly a third of the cases reported in this group.


The number of hepatitis A cases increased by 45 to reach 590 in the 20th week of the year. This is almost 2.5 times higher than at the same time in 2022, which was the previous record.


Cover image (for illustration purposes only): Getty Images








