Gergely Röst : COVID-19 vaccines are no panacea, comprehensive protection is needed

SARS-CoV-2 has claimed 4.5 million lives globally so far, but according to some estimates as many as 15 million people died of coronavirus-related diseases, said Röst. In terms of mortality this is the 8th most devastating pandemic in the history of mankind, he added.
Since the coronavirus outbreak, the spread of the Alpha variant (UK or Kent variant) was a key factor that was able to kick off the third wave. The next milestone was the first favourable trial results of Pfizer’s vaccine (in November 2020). The current challenge is posed by the Delta variant that is responsible for starting the fourth wave of the pandemic around the world, Röst gave a concise history of COVID-19.
He has also explained how an infection can become a global pandemic. He presented examples from the past, showing charts on various infectious diseases (influenza, Ebola, MERS, SARS, etc.), with their reproduction number (R0) on one axis and their severity (mortality) on the other. The ‘specialty’ of coronavirus is that the pandemic was caused by a combination of its high reproductive rate and severity.
Röst, Department Chair of the Applied and Numerical Mathematics Department at the University of Szeged, also stressed that due to the various methodologies used to calculate COVID-19 mortality it is worth looking at excess mortality data if we want to find out what the pandemic caused in different parts of the world.
Over the past 31 days, 1.3% of people diagnosed with COVID-19 have died, which compares with 0.7% a year ago when the ratio worsened later on, and we don't see a reason why it would not happen again this time.
Whereas the daily mortality figures may suggest otherwise, the cumulated data show that we're not better off than a year ago when there were no vaccines available. August was clearly worse this year than in 2020 in terms of total Covid deaths. September started off worse and showed improvement by the end of the month, but the balance of August and September shows that the situation in terms of Covid fatalities is actually the same as it was a year ago (167 deaths in Aug-Sept 2020 vs. 163 in 2021).

Even though vaccines were not in use a year ago and we have them now, the situation in terms of hospitalisation and ventilation should not be half as bad as it was last year. We can also hope that some cross-immunity exists to some degree at least, but with the new Delta variant and with this many people in hospital it might be a pipe dream.
The most likely explanation is that unvaccinated people make up the majority of severe cases, but authorities do not disclose the number or percentage of vaccinated and unvaccinated people among the infected / hospitalised / ventilated people.


Key takeaways
In his presentation, Röst has shown several key lessons learned from the pandemic:
The world was not prepared for such a pandemic, partly because critical infrastructure and institutions have recently been weakened or dismantled, and no country was aware of the real danger of such an outbreak.
Measures aimed to reducing contacts worked and they put a stop to the spread of coronavirus.
These measures come at a price, though. They have not only economic but also social repercussions, including impacts on education.
The fourth lesson is that the response to societies to lockdown measures is also of key importance. It matters a lot how acceptive people are towards restrictions and how willing they are to comply with these. It was proven over the last few months that new variants can trigger new waves, and restriction measures that had worked well before might not do the trick anymore.
Vaccines must not be regarded as panacea. They will not solve the problem overnight.
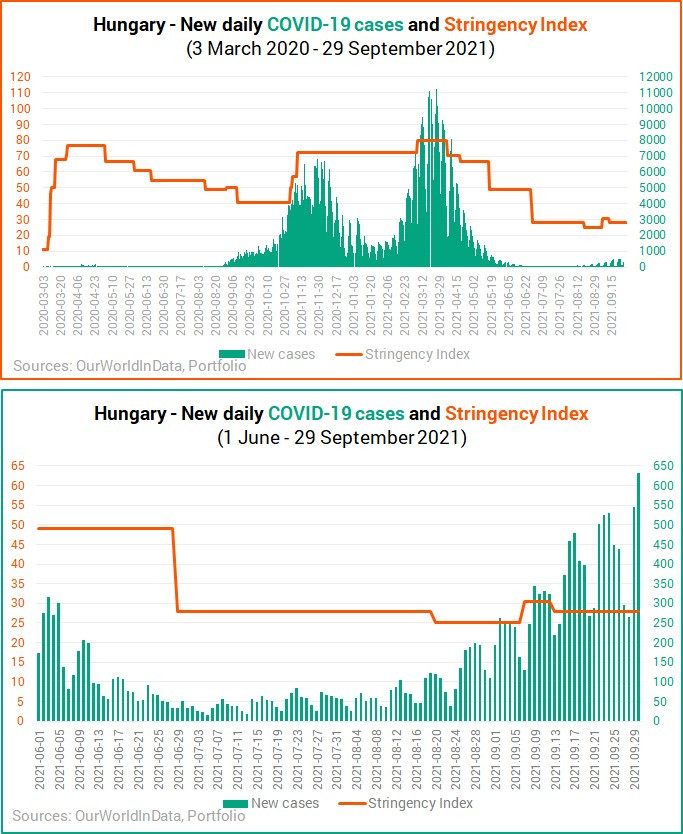
The other, non-pharmaceutical forms of protection must not be given up. A comprehensive programme of defense needs to be applied, as the various measures are mutually reinforcing. (We should note at this point that despite Röst’s recommendation, the Hungarian government is focusing almost exclusively on vaccinations, relying solely on jabs as The Solution. It lifted various lockdown measures in mid-May and then further eased restrictions in late June. Despite a rising number of new COVID-19 cases, hospitalisations and deaths, it has no intention to tighten anti-pandemic regulations. Note that Hungary scores 27.78 on the Stringency Index ( a composite measure based on nine response indicators including school closures, workplace closures, and travel bans, rescaled to a value from 0 to 100, with 100 being the strictest), versus 40.74 a year ago.
You cannot single out specific countries to serve as the ‘laboratory’ for Hungary. The epidemiological situation varies by country. The trajectories and social responses are different. If we focus too much on a single country, it could lead to a misguided strategy.
There needs to be a shift in paradigm on how we prevent and manage epidemics. Röst mentioned the recent opening of a World Health Organisation (WHO) office in Berlin (Hub for Pandemic and Epidemic Intelligence) as a positive example that indicates we need to have a new and different approach on how pandemics occur. Mathematical modelling needs to be incorporated into decision making processes. This, he said, would reform the whole system of disease control and prevention (data collection, data quality, real-time data, modelling, a constant teaching of the model), and the epidemiological surveillance system also be enhanced. He mentioned the United Kingdom, Australia and Canada as positive examples. The team he leads has been actively co-operating with the Ministry of Innovation and Technology and come up with several key analyses and prognoses.
What does the future hold?
In the short term (autumn and winter outlook), the following factors will determine the pandemic wave in Hungary:
- Vaccination coverage and particularly the vaccination coverage of the most vulnerable groups (e.g. elderly people)
- The vaccine portfolio and composition. Data of countries using different vaccines can vary due to this factor.
- Level of cross-immunity gained in previous waves.
- Sustainability of non-pharmaceutical protection measures (e.g. mask-wearing, social distancing, etc.).
- School and university education (in-class vs. distance learning).
- The efficiency of testing, contact tracing, isolation (quarantining).
- Uncertainties caused by the Delta variant.
- Immunity trajectory. There are signs in Israel, the United Kingdom and in the United States, as well, that the efficacy of vaccines wanes with time.
- Administration of the so-called booster shots, i.e. third doses.
- A potential emergence of new variants.
- Röst said the uneven distribution of vaccines in the world was a huge challange. There are severe vaccine shortages in various countries, while Western countries have such an abundance of COVID-19 shots that there’s a lot fewer people that are willing to get their jabs than vaccines.
As regards the longer-term outlook, Röst does not believe coronavirus will be eradicated. He thinks the most likely scenario is that
it will stay with us permanently, turning into an endemic, and recurring in a seasonal pattern.
This practically means that everyone will get infected, or even contract coronavirus multiple times. That is why it is paramount to be vaccinated in advance. Röst stressed that the severity of the virus will not diminish globally because this is its nature, but because the immunity of the population increases.
As regards long-term scenarios, there are two opposing beliefs among virologists, epidemiologists and other experts of the field:
- Under a highly optimistic scenario, the global population will build up serious immunity against coronavirus that will thus transform into a common contagious disease, and there will be spikes in new cases mostly in the autumn and winter.
- According to a lot more pessimistic scenario, the virus will continue to cause severe diseases and will come in waves.
This suggests that booster shots will be constantly needed in the future.
Röst also thinks we can identify various risks that could change our current view of the pandemic to its very core:
new vaccines, new therapies, new diagnostic procedures and/or new variants.
Cover photo: MTI/Péter Komka








